
Arthritis – Symptoms, Consequences, and Treatment Options
Osteoarthritis is a pathological, degenerative joint wear. The disease usually manifests through joint pain and minor discomfort, but if left untreated, it can lead to serious damage to joints and surrounding bone tissue over time. Inflammatory secondary diseases like arthritis can significantly reduce the quality of life for those affected due to severe pain and movement restrictions.
Osteoarthritis is the most common joint disease in the world – in Germany alone, around five million people are affected. So far, the disease is considered incurable, but it can be treated in various ways. If detected early and properly treated, the progression of osteoarthritis can be effectively slowed down. Additionally, you can integrate various measures into your daily life to counteract the onset or progression of osteoarthritis.
In this article, we focus on osteoarthritis and provide information on symptoms, possible causes, as well as common treatment and preventive measures. Here is an overview of the topics – simply click on the section you wish to read, and you will be redirected directly:
- What is Osteoarthritis and what variants can occur?
- Overview of Gonarthrosis, Coxarthrosis, and other types of Osteoarthritis
- What symptoms indicate osteoarthritis?
- Ways to diagnose osteoarthritis
- How can you prevent osteoarthritis?
- Activity instead of avoidance – Sports & Exercise against Osteoarthritis
- The right diet for osteoarthritis
- How is osteoarthritis treated?
- Conservative osteoarthritis therapy with movement and targeted stimuli
- Medication treatment for osteoarthritis
- Surgical interventions, joint prostheses, or joint fusion
- Conclusion
What is Osteoarthritis and what variants can occur?
Osteoarthritis is a disease that causes accelerated wear of joint cartilage – much faster and earlier than would correspond to the age of those affected. It is called a degenerative disease because the degraded cartilage tissue does not regenerate and with the progression of osteoarthritis, the surrounding joint bones are also affected.
Excessive strain – for example, from heavy physical work, obesity, or poor posture can accelerate cartilage wear and trigger osteoarthritis. Joint injuries can also reduce or damage the existing cartilage mass and promote osteoarthritis. Infections caused by bacterial infestation or joint damage resulting from inflammatory rheumatism are considered other possible triggers. Since joint wear usually progresses over a long period, older people are mainly affected by osteoarthritis. Women suffer from the disease more frequently, but on average at a higher age than men.
Lack of or one-sided movement plays an important role, as joints need to move to supply the cartilage tissue with nutrients. A knee that is stretched and bent daily through movement is statistically less susceptible to knee osteoarthritis than a knee that remains in the same position under the desk every day. Unmoved and completely unstressed, joint cartilage can literally dry out and roughen. This also increases the risk of injury, as under-nourished cartilage tissue can become brittle, like a gummy bear that you stretch. Unfortunately, cartilage tissue cannot heal such damage on its own. You will learn more about how important movement is to protect your joints from gonarthrosis, coxarthrosis, and other types of osteoarthritis later.
The known triggers of osteoarthritis are divided into primary and secondary types. Primary osteoarthritis refers to diseases favored by genetic predisposition, which essentially means that affected individuals have an increased likelihood of developing the disease. Non-genetic or lifestyle and external influences triggered disease causes are referred to as secondary osteoarthritis. Here are some possible triggers for secondary osteoarthritis:
- Excessive or one-sided strain on the joints due to obesity, hard work, or as a result of accidents.
- Joint misalignments – congenital, caused by poor posture, or as a result of accidents.
- As a result of other diseases that affect the joints, such as gout or rheumatoid arthritis.
- As a result of diseases or unhealthy habits that affect metabolism and blood circulation. For example, diabetes mellitus can increase the risk of osteoarthritis. Various joint inflammations can also damage the joint cartilage.
- The side effects of some medications could promote osteoarthritis – for instance, gyrase inhibitors are suspected of damaging the connective tissue around the joint cartilage and contributing to a faster breakdown of cartilage tissue.
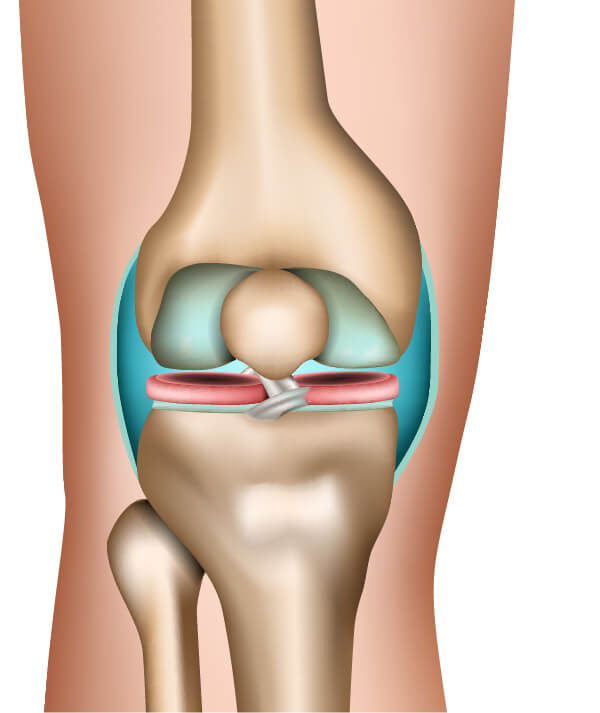
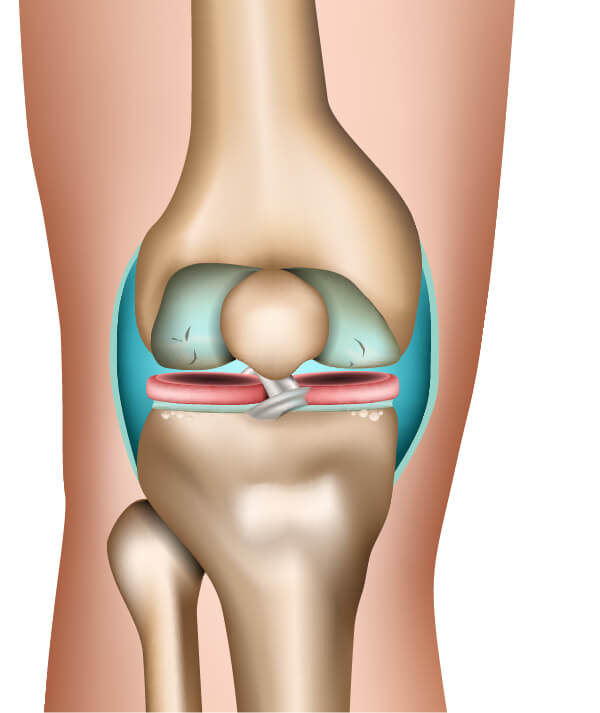
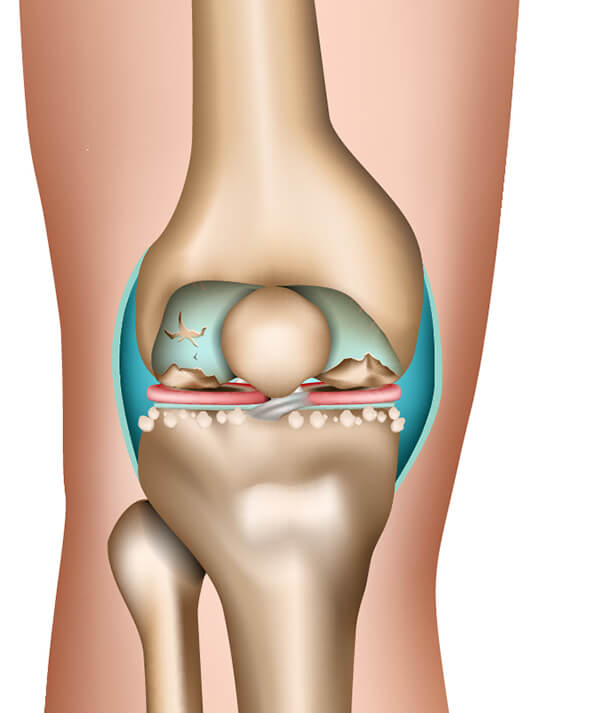
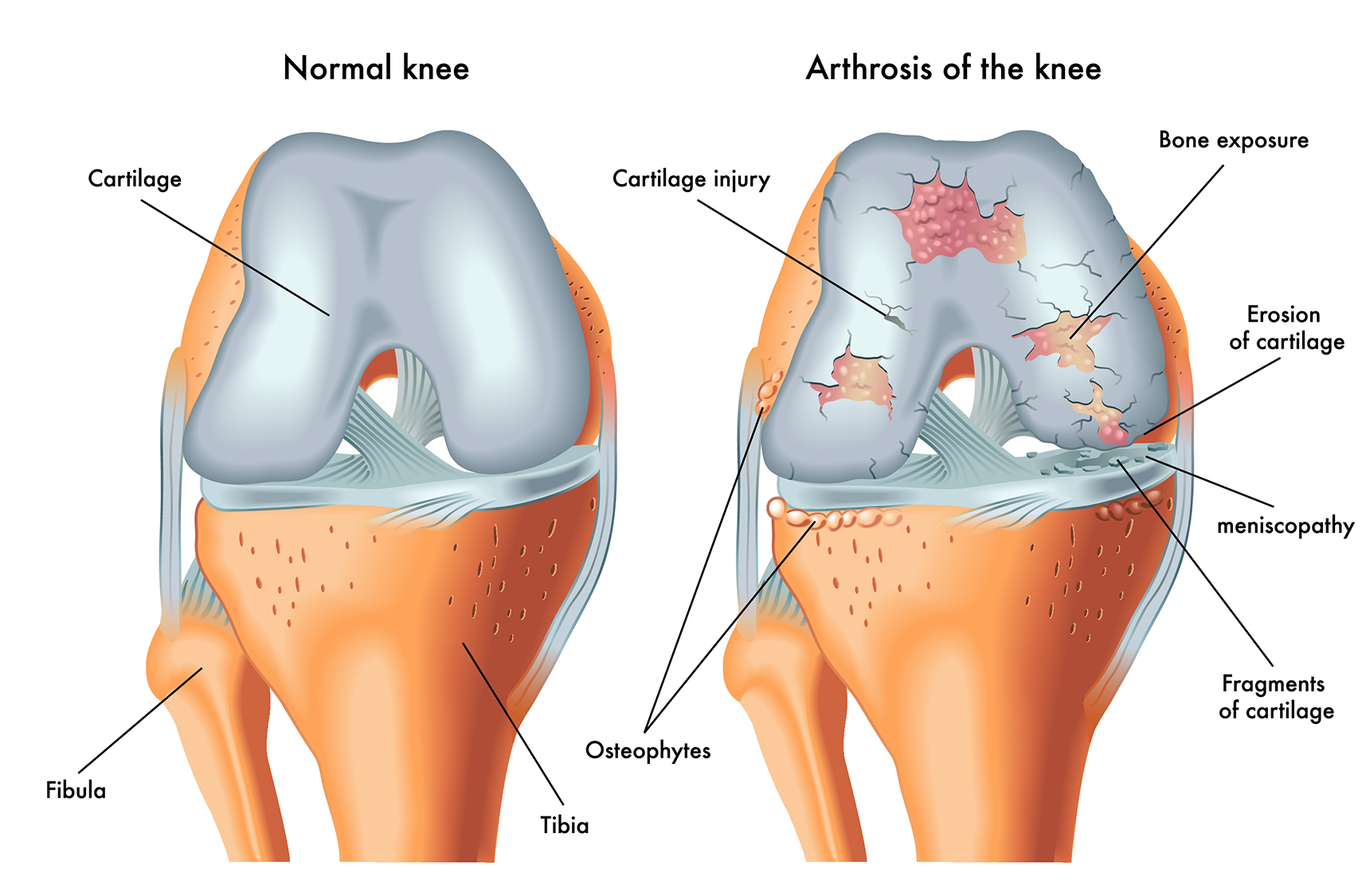
While early-stage osteoarthritis initially causes mild symptoms, severe late effects occur if the disease is ignored or not recognized. In a healthy joint, the ends of the bones that meet – the joint head and socket – are covered by a protective layer of cartilage. The joint is enclosed by a joint capsule filled with joint fluid, which acts like a lubricant on the joint cartilage. If the cartilage layer gets cracks or recedes, bone increasingly rubs against bone.
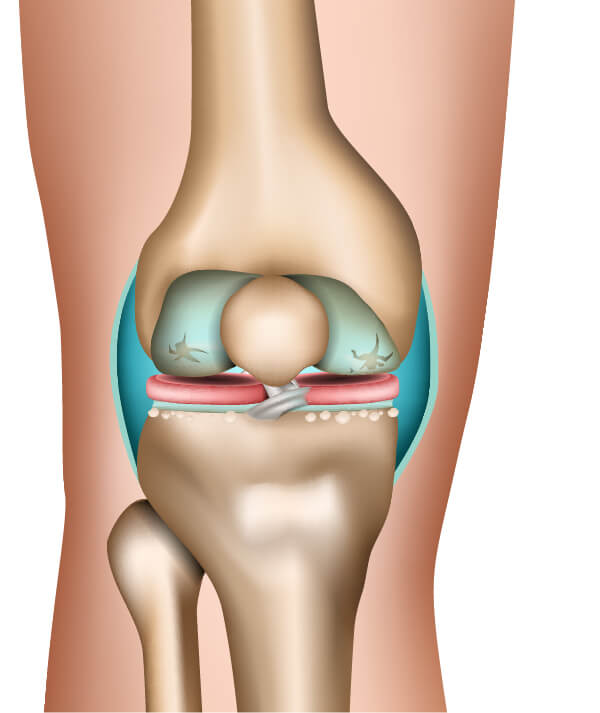
The more the cartilage layer is destroyed by osteoarthritis, the more pain is caused by the direct contact of the joint bones with each movement. Worse yet, over time, the pressure of the joint head on the socket can lead to bone deformities. The joint head presses into the socket – in advanced stages, narrow bone spurs form on the sides of the joint socket. These bony protrusions are called osteophytes. These deformities can severely restrict the joint's mobility.
In advanced osteoarthritis, fragments or fibers may detach from the damaged cartilage. These fragments move within the joint capsule, causing pain and irritation and even slipping between the joint bones, potentially blocking the joint. In the case of osteoarthritis in the hand, this could lead to the sudden stiffening of a finger joint.
The progression of osteoarthritis can be divided into several stages:
- In the early stage of osteoarthritis, the effects are still very minor. The joint cartilage begins to thicken and deform.
- Subsequently, the once smooth cartilage layer becomes increasingly uneven and starts to fibrillate.
- As the protective joint cartilage becomes thinner, the space in the joint gap also shrinks until the joint bones meet without the protective cushioning of the sliding film. First compressions and changes in bone tissue occur. The joint surfaces begin to flatten due to friction.
- In the late stage of osteoarthritis, the cartilage layer is sometimes completely worn away. Bony spurs form on the sides of the joint sockets, while the bone at the pressure points becomes highly densified. Affected joints are severely restricted in their mobility and function.
Overview of Gonarthrosis, Coxarthrosis, and other types of Osteoarthritis
Osteoarthritis can affect practically all joints in the body. In practice, however, it usually affects specific body areas. The condition often begins in the knees, hips, or fingers. The affected limbs were often subjected to one-sided stress for a long time. For example, if the knees are heavily strained throughout a working life, the risk of developing knee osteoarthritis in old age increases.
Depending on the strain on various body parts, beginning osteoarthritis in other joints may not be noticed because it does not yet cause symptoms. If multiple forms of osteoarthritis described below occur together, it is called poly-osteoarthritis.
- Gonarthrosis – Knee Osteoarthritis: Gonarthrosis is one of the most common forms of osteoarthritis. The knees carry a large part of the body weight and are also subjected to rotational and bending stresses. Ligament or cartilage injuries in the knee area are therefore among the most common sports injuries. For example, as a result of meniscus injuries, parts of the cartilage may need to be surgically removed. Knee osteoarthritis can be triggered by the consequences of injuries or long-term wear in the knee joint. Misalignments such as bowlegs or knock-knees are also believed to promote gonarthrosis. As knee osteoarthritis progresses, it eventually affects the bones in the upper and lower legs over time.
- Coxarthrosis – Hip Osteoarthritis: Wear and tear of the hip joints often lead to coxarthrosis in old age. In addition to excessive strain, various hip disorders that lead to joint deformities are considered risk factors for hip osteoarthritis. Diseases such as Legg-Calvé-Perthes disease or hip dysplasia can be congenital or occur in childhood and only lead to coxarthrosis many years later.
- Finger Osteoarthritis: Various joints in the fingers can also be affected by osteoarthritis. In addition to the effects of injuries or very hard work, it is often seen that fingers are particularly prone to damage from poor posture and the effects of monotonous office work. Finger osteoarthritis can also result from permanent underuse – when typing on the keyboard, the joints remain in the same position for a long time and are not moved enough to be adequately nourished with nutrients. The most common forms of finger osteoarthritis include thumb osteoarthritis (rhizarthrosis), which affects the thumb base.
- Spondylarthrosis – Spinal Osteoarthritis: Our spine owes its mobility to small joints that connect the individual vertebrae. These joints are subjected to high stress throughout life, making spondylarthrosis one of the most common forms of osteoarthritis in old age. The degree of spinal stress is important – jobs that involve carrying heavy loads carry a higher risk of developing spondylarthrosis. The disease often accompanies disc problems. In addition to physical strain or poor posture, obesity is also a risk factor for spinal osteoarthritis.
- Omarthrosis – Shoulder Osteoarthritis: The shoulder joint often has to bear heavy loads. Because it is a highly mobile joint with high rotational capability, the risk of shoulder injuries is also high, especially if overloaded in an unfavorable position. Incorrectly performed sports exercises with weights can also lead to wear of the joint cartilage or damage to tendons and ligaments. Omarthrosis often develops as a late consequence of shoulder joint injuries. Rheumatism is also considered a possible cause of shoulder osteoarthritis.
- Osteoarthritis in Feet and Toes: Since our entire body weight rests on the feet, it is not surprising that they are prone to osteoarthritis. Obesity is an important factor, but unsuitable footwear also plays a role in their development. Osteoarthritis often occurs in the big toe's metatarsophalangeal joint. The ankle joints are also frequently affected, as they absorb our body weight with every step and are subjected to high wear.
- Osteoarthritis in Hands and Arms: Hands and fingers perform diverse and complex movements. Injuries or overuse can increase the risk of osteoarthritis in the numerous small joints and cartilage. It has also been shown that underuse in the hands can increase wear. For example, office work like typing, where hands and fingers remain in a few positions and only perform monotonous movements, leads to reduced nutrient supply to the cartilage tissue. Finger osteoarthritis can occur in all finger joints, but usually starts with one or a few joints. The thumb joint (rhizarthrosis) is also often affected. Arthritic finger joints swell significantly over time, making this form of osteoarthritis also very noticeable. Osteoarthritis in the arms can occur in the wrist as well as in the elbow joint.
- SIJ Osteoarthritis: The sacroiliac joint connects the sacrum and ilium – located in the pelvic area. These joints absorb a good portion of the forces acting on the pelvis during hip movements. SIJ osteoarthritis, which affects these joints, is one of the most difficult variants to treat.
- Temporomandibular Joint Osteoarthritis: Hardly any joint moves as much over a lifetime as the temporomandibular joint. Therefore, osteoarthritis can also develop there – especially in old age.
What symptoms indicate osteoarthritis?
Since osteoarthritis develops very slowly, it is often recognized late. Many early symptoms can also be caused by various other conditions, injuries, or unusual strains. Sometimes, the development of osteoarthritis seems to slow down over longer periods, so that those affected get used to occasional pain and miss the early detection of the joint disease.
In the initial phase, osteoarthritis announces itself through pain, stiffness, or a feeling of tension in the joints. Those affected by gonarthrosis often complain of knee pain when the weather is damp and cold. It is particularly noticeable when the pain is most severe when starting movement and then slowly subsides. These are called start-up pains.
If osteoarthritis is still in its early stages, the pain is usually only noticeable when the joints have to absorb shocks. Osteoarthritis in the knee, for example, would be noticeable when jumping or descending stairs.
Changes in gait or movement restrictions are other warning signs of osteoarthritis. Coxarthrosis, for example, makes it difficult for those affected to bend forward and tie their own shoes.
Over time, swelling appears on affected joints. The pain no longer subsides even at rest. Those who suffer from severe osteoarthritis often have trouble sleeping peacefully at night. If the joints feel noticeably warm to the touch, this can indicate inflammation in the tissue. These complaints can be caused, for example, by detached cartilage material or abraded bone fragments. There is also the risk that such inflammations will lead to secondary diseases.
In the late stage, osteoarthritis often leads to disability and significantly impairs the quality of life due to extreme pain. Osteoarthritis in the fingers and hands, for example, can lead to joint deformities that make it impossible to grasp and hold objects.
If you believe you may have osteoarthritis, you should definitely have this suspicion medically clarified. Doctors have various options to prove the disease or to assess how high your personal osteoarthritis risk is.

Ways to diagnose osteoarthritis
How can osteoarthritis be detected? Joint pain can also arise from minor injuries or other diseases like gout. The diagnosis thus begins with a thorough questioning of the patients. It is important to clarify exactly when the pain occurs. The start-up pain is a sign that can indicate osteoarthritis. Additionally, the life circumstances of those affected are examined. What strains exist in everyday life and work, is competitive sports practiced, or is there a history of previous injuries or surgeries?
The affected joints are palpated to look for swelling or deformities. An accurate diagnosis is usually only possible using imaging techniques. Modern medicine offers various technologies for osteoarthritis diagnostics:
- X-rays: X-ray images show bones very clearly and in great detail, while softer tissue is difficult to see. Through X-rays, joints can be examined for misalignments, deformities, and damage. A severely narrowed joint space, for example, is a clear indication of osteoarthritis. If necessary, more elaborate procedures can be used to verify the diagnosis.
- Computed Tomography: CT is also an X-ray procedure. Patients are placed on a couch that slides into a scanning tube. Numerous X-ray images are taken in this tube, which can then be layered to create a highly precise image of the affected joints.
- Magnetic Resonance Imaging: Also known as MRI, this is an imaging technique without X-rays. The technology is new and more expensive than simple X-rays. However, both the bones and the surrounding tissue can be examined precisely. This examination also takes place in a scanning tube.
Since these modern diagnostic technologies are available, physical examinations where the joint is surgically opened are hardly performed anymore. The infection risk with such procedures is simply too high. The only exceptions are minimally invasive procedures like aspiration, where joint fluid is extracted for laboratory analysis, or arthroscopy – the so-called joint endoscopy.
Arthroscopy is performed using an arthroscope – a special endoscope. It is a medical probe equipped with a camera, a light, as well as irrigation devices or medical grasping and cutting tools. However, due to modern non-invasive procedures, arthroscopy is now less used for diagnosing osteoarthritis and more for treating symptoms. For instance, detached cartilage fragments can be removed with the arthroscope.

How can you prevent osteoarthritis?
As we age, the risk of developing osteoarthritis increases – making it all the more important to take preventive measures as early as possible. Even if you belong to risk groups with incurable diseases like diabetes mellitus, you can contribute significantly through your lifestyle to avoiding osteoarthritis or only developing it at an advanced age.
Activity instead of avoidance – Sports & Exercise against Osteoarthritis
When the joints hurt, many people tend to adopt protective postures and avoid exertion. But this is not the best method to counteract osteoarthritis. Regular movement is necessary for the joint cartilage to be supplied with nutrients and remain supple. Therefore, long periods of sitting contribute significantly to joint wear – although they are not stressed, they are not nourished either. Inactive joints "dry out" as a result. This also reduces the cartilage tissue's resilience and increases the risk of injury.
If you want to exercise to prevent osteoarthritis, it is advisable not to train too much and not too little. Especially if you have been inactive for a long time, you should start your training gently and with light exercises. You essentially have three important goals:
- Move the joints to ensure the joint cartilage is adequately supplied with nutrients.
- Train the muscles to provide better support for your joints. All joints are surrounded by muscles that absorb a good portion of the forces acting on the joints.
- Prevent or reduce overweight – many types of osteoarthritis, such as gonarthrosis or coxarthrosis, are promoted by high overweight. Every excess kilogram increases the pressure on the joints that carry the body weight.
Suitable sports for osteoarthritis prevention are those where joints are moved but not overly stressed:
- Swimming: Water carries a large portion of our body weight, so the joints are only minimally stressed when swimming. If you regularly swim a few laps in the pool, you are giving your whole body a valuable training session. Swimming movements also involve many small muscles in the movements.
- Water Gymnastics: Gymnastics can also be performed particularly joint-friendly in water. Therefore, water gymnastics is also recommended for already advanced osteoarthritis. Individuals with restricted movement or weakened by age can also train in the water without any risk of falling.
- Cycling: Pedaling is a smooth movement, with the weight load primarily on the bicycle saddle and not on the joints. Thus, the knees can move freely without pressure. Cycling mainly helps prevent gonarthrosis.
- (Nordic) Walking: The good old walking is still one of the best activities we can do for our bodies. Humans are naturally designed to cover long distances every day while walking upright. Walking – preferably at a faster pace – stimulates circulation and metabolism, uses and supplies muscles with blood, moves joints, and supplies them with nutrients. Even if osteoarthritis is already present, walking is important. For gonarthrosis or coxarthrosis, walking sticks can be used to distribute body weight additionally.
- Gentle Strength Training: Muscles can also be built up through targeted strength training, where individual muscle groups can be specifically activated. To train joint-friendly in osteoarthritis, exercise bands are recommended. With a fitness or resistance band, the load increases in proportion to the applied force. The joints are less stressed than in weight training. The weight of the dumbbell remains constant – a band adapts to your capabilities. Fitness and resistance bands can be ordered cheaply from the Medicalcorner24® online shop.
Avoid sports where the joints are exposed to high pressure or strong impacts. Squash is considered particularly harmful to the joints. Jogging can also do more harm than good to knees and ankle joints. Many people unfortunately do not jog on soft, resilient ground but on unyielding pavement. Even if you jog with ideal footwear on soft forest floors, you stress your joints more than if you walked quickly. Prefer walking or long walks if you want to protect your foot, knee, and hip joints.
If you have been diagnosed with osteoarthritis, you should first seek medical or therapeutic advice on which sports are suitable for you and which you should avoid. In many cases, tailored therapies for various forms of osteoarthritis can be recommended.

The right diet for osteoarthritis
It is suspected that diet has a strong influence on the development and progression of osteoarthritis. However, this influence is difficult to attribute to individual foods – it is more about which nutrients we consume and whether we consume too much or too little of them. One thing is certain: a diet that leads to overweight increases the strain on the joints and thus the risk of osteoarthritis. Furthermore, animal proteins – consumed in excess – are considered risk factors, as the omega-6 fatty acids they contain promote inflammation. Joint inflammations can lead to osteoarthritis.
How should one eat to prevent osteoarthritis? A vegetarian or vegan diet can provide the body with all essential proteins and nutrients without promoting inflammatory processes or causing overweight. Vegetables should make up the main part of meals – fruit, on the other hand, should be consumed in moderation due to its calories. Prefer cooking with vegetable oil rather than butter or animal fat.
Fish and other seafood, as well as various whole grain varieties, contain anti-inflammatory omega-3 fatty acids. Opt for whole grains and wheat and consider eating fish several times a week. Fish can also make the transition from a meat-rich diet easier. It is also advisable to avoid alcohol consumption and to quit smoking.
How is osteoarthritis treated?
Besides exercise and physical therapy to keep the joints moving and strengthen the muscles, various medicinal or surgical treatments are used against osteoarthritis. The goal of osteoarthritis treatment is to eliminate or alleviate pain and stop the progression of damage to cartilage and joints. Which treatment methods are suitable and how high the chances of success are also depend on the stage at which osteoarthritis is detected. So, it is better to get an orthopedic check-up one time too many than too few.
According to the current medical standard, destroyed cartilage tissue cannot be replaced or healed. As long as research does not provide a solution here (e.g., through laboratory-grown cartilage tissue), the treatment of osteoarthritis aims to stop the progression of the disease.
Conservative osteoarthritis therapy with movement and targeted stimuli
In the early stages of osteoarthritis – as long as enough healthy joint cartilage is still present – treatment can often still be conservative without the use of medication. Movement plays an important role. Depending on the patient's age and possibilities, sports, physical therapy, or physiotherapy can be used to keep the joints moving and nourish the remaining cartilage with nutrients. At the same time, the strain on arthritic joints must be minimized. In cases like gonarthrosis, coxarthrosis, or osteoarthritis in the feet, overweight is particularly harmful. Besides controlling body weight, harmful habits like smoking or excessive alcohol consumption should also be avoided.
Targeted movement therapy can help make already arthritic joints more mobile again. For coxarthrosis, gonarthrosis, or foot osteoarthritis, aids like walking sticks, canes, or walkers can be used to provide relief. Sports that place a high weight on the joints or require them to absorb impacts and shocks should be avoided.
Physical therapy can also help to relieve pain in osteoarthritis. From massages to mud and peat packs to the targeted use of heating pads, cherry pit pillows, or hot water bottles, there are various methods to improve blood circulation in the tissue. The heat also helps to relax muscles tensed by protective postures. In contrast, cold therapy is often used for severely affected or inflamed arthritic joints. The short-term, strong cooling of affected joints reduces swelling, alleviates pain, and aims to counteract inflammation.
If necessary, X-ray radiation can be considered. Short-term, targeted radiation is supposed to combat inflammation and stimulate blood circulation. Alternatively, magnetic field therapy for osteoarthritis is increasingly being used. The joint is exposed to a magnetic field – in the hope of stimulating metabolism, alleviating pain, and reducing swelling. However, the effectiveness of magnetic field therapy in osteoarthritis is not sufficiently scientifically proven.
Medication treatment for osteoarthritis
The treatment of osteoarthritis symptoms like pain or inflammation can be done with medication. Painkillers that come into question belong to the group of non-steroidal anti-inflammatory drugs (NSAIDs). Ibuprofen or diclofenac are examples of NSAIDs. However, long-term use of painkillers can have harmful side effects. Therefore, the intake of any medication should definitely be medically clarified.
Cortisone injections can calm severely swollen and inflamed joints. However, cortisone cannot be a permanent solution due to side effects. If cortisone is administered too often, it can negatively affect blood pressure, blood sugar, or cholesterol levels, among other things. Additionally, cortisone causes hunger attacks, which counteract weight loss efforts.
Hyaluronic acid injections are supposed to "lubricate" arthritic joints and thus stop or slow down the wear of the joint cartilage. Hyaluronic acid is actually produced by our body as a kind of lubricant for the joints. The method promises at least temporary relief from osteoarthritis. However, the injection itself is not without risk, as germs can enter the joint during the procedure and cause inflammation.

Surgical interventions, joint prostheses, or joint fusion
Surgery should always be the last resort – but in advanced osteoarthritis, surgery sometimes offers the last solution. Depending on the progression and type of osteoarthritis, different procedures can be used:
- Flushing or Sanitation: Minor procedures on the joints can be performed using an arthroscope. In the so-called lavage, a probe is inserted to flush the joint with a saline solution. This is supposed to remove tissue particles floating freely in the joint fluid, causing irritation. In the sanitation (debridement) of a joint, loose cartilage parts are removed, and rough joint cartilage is smoothed. Debridement can, for example, resolve cartilage fragments blocking the joint and improve the mobility of an arthritic joint.
- Cartilage treatments and cartilage transplantation: In recent years, new treatment approaches have been tested to partially restore damaged cartilage. It has already been possible to transplant cartilage tissue from healthy joints to "repair" worn joints. Another method involves fine drilling into the affected joint cartilage to stimulate the tissue to "fill in" the gaps.
- Operative correction of the joint: Osteoarthritis is often caused or promoted by the misalignment of a joint and the associated uneven load. In the so-called correction osteotomy, the joint bones are surgically realigned. This procedure is also performed prophylactically to correct joint misalignments before they cause serious problems.
- Joint prostheses: The development of joint prostheses has made significant progress in recent decades. If osteoarthritis is so advanced that other treatments no longer provide relief, it may be considered to partially or completely replace the joint. Not all body joints can yet be replaced in this way. For gonarthrosis or coxarthrosis, prostheses have already proven effective in replacing arthritic knee or hip joints.
- Joint fusion: If a joint prosthesis is not an option, joint fusion (arthrodesis) can be considered. Here, the arthritic joints are removed, and the ends of the bones are firmly connected. This removes the source of pain but also significantly restricts the mobility of the affected limb. Arthrodesis is most commonly used in the finger and wrist area.
Conclusion:
Can osteoarthritis disappear again? According to the current medical standard, the answer is no. However, diagnosed osteoarthritis can be treated, slowed down, and possibly even stopped. Furthermore, you can take many measures to protect yourself from joint wear, prevent osteoarthritis from occurring, or delay its onset into old age.
The symptoms of osteoarthritis can be partially compensated for by aids. If it is difficult for you to open jars and bottles due to osteoarthritis in the fingers, for example, you can use a universal opener. Dressing aids can make dressing and undressing easier if hands, elbows, and shoulders are restricted by osteoarthritis. In the Medicalcorner24® online shop, you will find many products that can make daily life easier for you in case of movement restrictions.



